The Future of ACL Resilience Remains Hidden within the Complex Sensorimotor System
This blog was written for ACL Study Day (Evidence and Practice, formally known as Southcoast Seminars)
The hard truth about ACL rehabilitation
Our treatments fail to adequately restore self-reported knee function, prevent subsequent injury, and stave off post-traumatic osteoarthritis. Relatedly, our largely pre-planned rehabilitation techniques and test batteries have questionable validity when it comes to preparation for the chaos of sport. As clinicians and scientists, the sooner we accept these facts and recognize the complexity of this problem, the sooner we can solve it. No one thing can fill this gap. Instead, we need to consider the many interwoven domains of health and sport. The purpose of this post is to outline the complexities plaguing ACL injury and recovery and to begin a dialogue between the clinicians and researchers charged with developing the future of ACL rehabilitation.
More than biomechanics
ACL injuries occur due to biomechanical faults (e.g., excessive knee valgus, etc.), right? Well, sort of. As Dr. Chaput and Harjiv Singh previously discussed in this blog post, these injuries are products of complex non-linear systems failure. Biomechanical faults are necessary, but not sufficient to cause injury in isolation.
Sport is a complex system. The final score is determined by the relative skill and performance of individual players, how each player and coach interact with teammates, the ever-evolving dynamics of the game (e.g., substitutions, crowd noise, refereeing, etc.) and the elimination of time on the game clock. The two interacting teams are rarely “perfect”, but each adapt to faults in order to score points, maximize possessions, and win. This feature of adaptation is true of all complex systems: despite obvious flaws, the complexity allows for variability in the way the systems run. In this regard, biomechanical faults are a “minor flaw” of human movement and do not always result in injury. Could natural biomechanical variability be the scapegoat of wider systems failure? Consider the implications.
Navigating sport
In sport, two interacting adaptive systems (i.e., teams) interfere with the others’ effectiveness in scoring points. This contributes to the evolution of the larger system (i.e., game) over time. Ultimately, the motor options available to individual athletes are dependent upon the dynamics of the environment, task, and organism; all of which influence how the task is able to be completed. Suggesting that the presence of a biomechanical fault can singularly determine an athlete’s injury risk is implausible as this fails to account for these inter-personal dynamics. Figure 1a and 1b. So how can we take this into account?
Inter-personal dynamics
More than two-thirds of ACL injuries occur from noncontact mechanisms, many of which are associated with collision avoidance,1,2 such as a point-guard cutting to avoid a defender. Anecdotally, many of us believe the inter-personal dynamics of sport contribute to ACL injuries; they tend to occur more frequently in game play than practice2 and to defenders than offenders.1 However, foundational questions remain. Do individuals at risk for (or following) ACL injury perform worse at reactive inter-personal coordination tasks? Can this be optimized through training? If so, how?
There are currently no investigations into inter-personnel dynamics surrounding ACL injury or return to play. Still, the realization that opponent actions disrupt movement patterns3 threatens the validity of traditional rehabilitation. Are we effectively developing readiness for sport? A deeper understanding of our patients’ adaptability to environmental perturbations (and how to optimize it) is an area of much needed research. Enter: the sensorimotor system.
Brains and sprains
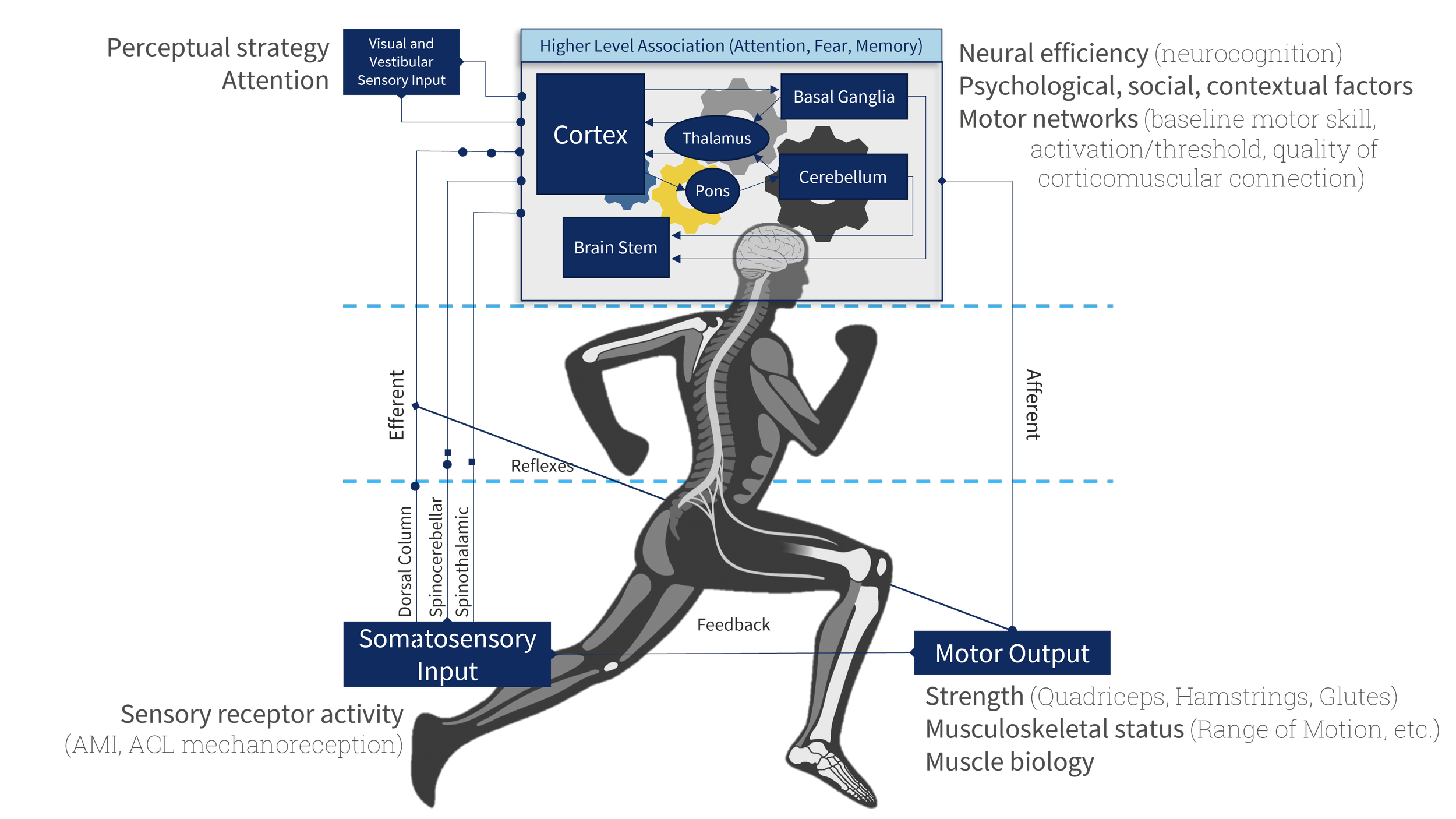
The brain is the director of sensorimotor control. Research in the past two decades has popularized the fact that sensorimotor control determines the behaviors and biomechanical faults contributing to, or resulting from, ACL injury. The sensorimotor system is embodied within the rapidly changing environment. A deeper look into the complex mechanisms influencing musculoskeletal rehabilitation will help to define the scope of the problem. The following sections are just an introduction to the many interconnected features of sensorimotor control we’ll need to consider.
The sensorimotor system is a feedback loop.
Our central nervous system (CNS) continuously integrates sensory information from multiple modalities (visual, vestibular, somatosensory, auditory, etc.) to construct a representation of the environment. Subsequent motor actions change sensory input, and the cycle continues. Without feedback, successful motor behavior is not possible.4
Under the surface, the sensorimotor system must first distinguish between stimuli generated by the environment from predicted feedback generated by our own behaviors.5-7 Impairments in sensory inputs or sensory weighting (e.g., visual dependence) may influence the accuracy of this environmental vs. self-afferent distinction, and are the basis of claims that sensory and motor prediction errors contribute to ACL injury.5,8 When considering how individual variability and impairments might influence sensorimotor feedback loops, intra-personnel coordination (i.e., the ability to control our body’s in space) becomes just as complex as the dynamics of sport.
Intra-personnel dynamics
Consider a point guard trying to shoot a layup. As they move toward the net, the sensorimotor system is charged with controlling infinite degrees of freedom while perceiving the evolving environment. Such athletic actions require coordination of distributed groups of muscles and joints. A few studies9-11 investigating this concept in individuals with ACLR characterize less adaptability of joint coordination during single-limb balance,9 with higher rigidity indicating higher re-injury risk.10 The same pattern of less variable joint coordination is true of gait as well.11 Unfortunately, these impairments are less clinically tangible than muscle weakness or range of motion restriction. What modifiable factors contribute to these impairments? How can we be sure we are addressing them?
Disruption of sensory afferent feedback at the knee joint, differences in perceptual and cognitive processing, and subsequent alterations in muscle recruitment are all thought to influence intra-personal coordination. As we journey through the sensorimotor system, remember: sensory input and integration inform motor output.
Somatosensory afference: What happens to ACL mechanoreceptors after injury?
Proprioception is generated by receptors within ligament, capsular, and musculotendinous tissues throughout the body. As we know, these signals allow perception of body positions, movements, and muscular effort.12,13 Integration of this diverse and distributed array of somatosensory afference is incredibly complex, including spinal cord, cerebellar, and higher-order CNS centers.12,13
The ACL and surrounding knee joint structures constitute the largest sensory organ in the human body.14 Neuroscience simply doesn’t yet have the techniques to describe what is encoded in afferent signals, but the presence (or absence) of signal is informative of function after ACL injury. Individuals without ACL afference upregulate hamstrings stiffness and activity, thereby creating active stability.15 Conversely, those with preserved ACL afference after ligament rupture do not upregulate hamstrings activity, and tend to be non-copers.15 Although still unclear, patients may recover ACL afference in the long-term after ACLR with ligamentization of the grafted tissue.16 Regardless, considering all individuals who undergo ACLR were at one time ACL deficient, the status of this pathway continues to have functional and clinical implications “up the (sensorimotor) chain” but is largely unknown or unmeasured in the early post-operative stages. Are there clinical signs that can help us?
The role of integrative cortices and neurocognition
It seems that periods of deafferentation after ACL injury are enough to catalyze long-term neuroplastic changes in the brain, and functional differences in brain activity exist prior to injury.
After initial integration in the spinal cord, sensory signals transmit to the brain where sensory integration helps to predict the emerging environment.7 An athlete must use perceived information to make hundreds of motor decisions during a game.
Key to this success is the athletes’ ability to deliberately search for, interpret, and predict relevant information pertaining to the current and future dynamics of the task and environment. In other words, performance is constrained by the situation, the athletes' physical capacity, and their perceptual-cognitive control.18 For example, individuals who go on to suffer ACL injury have slower neurocognitive processing speed and visuomotor reaction time preceding the injury.19 These impairments likely persist (and worsen) after injury. So, can we train it? If so, are we?
Neural efficiency in athletes
Neural efficiency is the ability of one individual to integrate more perceptual-cognitive information than another, assuming a ceiling of neural capacity.20 This means, among other things, more information-processing, more effective motor actions, and more activity in sensorimotor areas of the brain.21
Neural efficiency is shown with higher intelligence,22 musical ability,23 and isolated motor skill.20,24 In all domains, experts require less neural activity for a standardized task. However, when in complex environments, such as sport, experts use more neural activity, not less. For example, highly skilled players show greater activation of the mirror neuron system than low skilled players while predicting opponent's movements25 or analyzing movements.26 These results suggest that incremental reductions in cortical demands of isolated tasks allows experts to process more information and better navigate the complexity of sport.
Future research should investigate the utility of rehabilitation and coaching methods in best developing neural efficiency and its association with skill acquisition. For now, findings of increased fMRI activity in visual and attentional networks during simple rhythmically paced tasks indicate neural inefficiency after ACLR.27 Suggesting an opportunity for neuromodulatory interventions aimed at neurocognition and integrative networks.
Attention!
In general, attention selectively prepares the cognitive system for the differentiation between relevant and irrelevant features of the environment. A growing library of research suggests goal-directed attention (termed external focus) results in improved performance compared to self-directed attention (termed internal focus),28 with implications for ACL rehab reviewed in detail elsewhere.29,30 Results suggest external focus of attention facilitates ability to plan, select, and execute an action with improved perception of the environment, whereas internal focus of attention disengages perception from the surrounding environment.
Following ACLR, fMRI findings suggest greater cognitive demands during rhythmic motor tasks.27 Further, healthy individuals at high risk for ACLR injury demonstrate less variable cortical activity31 and cortical signs suggestive of less adaptable motor coordination.8 Although the connection is still theoretical, attention-based neuromuscular training strategies do target these suboptimal cognitive-motor strategies.28,32
But is it all solved with neurocognitive training?
What else goes on in our heads?
The neural processes of the limbic system (emotion & memory) are intricately intertwined in motor behavior. Neuroplasticity in this system is theoretically linked to negative behavior change in low back pain and chronic pain models, and has been extended to the ACLR population.30 Meaning we must consider the influence of motivation, fear, anxiety, pain, memory, etc. on our athletes’ motor control.
A few recent papers33,34 highlight a wide range of psychological, social, and contextual factors that influence our patients’ recovery following a traumatic knee injury. Critically important to psychological and societal health and well-being, psychological factors have also been directly linked to quadriceps function35 and reinjury rates after ACLR.36 Psychological, social, and contextual factors evolve over recovery stages and should be considered priority in managing individuals following ACLR.
3 sets of 10 is not gonna cut it
The basal ganglia and the interconnected motor cortices are implicated in action selection, initiation, and task-switching. As clinicians we focus on largely pre-planned and deliberate motor acts – so patients get good at using this “3 sets of 10” motor system (i.e., supplementary motor area). Yet, differences in neural activation between controls and individuals with ACLR suggest a reduced propensity for reactive motor control.27
Reactive movement is likely more important for sport, and uses a different motor system (i.e., premotor areas). This suggests a need for therapeutic exercises (and research paradigms) that focus on reactive motor planning in complex/changing environments. Head back to this blog post for some ideas.
“All or none” is bit harder to come by
The descending corticospinal tract is responsible for initiating voluntary muscle contractions and regulating descending motor control. As with any neuronal pathway, the balance between excitatory and inhibitory potentials influences transmission and “all or none” motor neuron activation. Reduced excitability of the corticospinal tract after ACL reconstruction means more activation is required prior to initiation of movement. Despite treatment, this impairment gets worse over time37 and the tract itself appears to atrophy.38
Furthermore, corticospinal excitability is strongly associated with key features of quadriceps muscle function (e.g., rate of torque development39) and thus functional recovery. To this end, we need to develop and adopt treatment strategies that increase corticospinal tract excitability.37 EMG biofeedback,40 motor imagery,41 and eccentric exercise are promising avenues.
Finally, the muscle itself
The primary clinical feature of individuals with ACLR is quadriceps muscle atrophy.42,43 As clinicians we battle persistent quadriceps inhibition,43 atrophy,42 and weakness.
Decoupling of nervous tissue and the muscle (known as denervation) severely limits the ability to volitionally contract muscles, increases intramuscular fat deposits, catalyzes fiber type transitions, increases circulatory atrophy mediators, and lowers satellite cell counts.42 Treatments such as blood flow restriction and eccentric exercise are mechanistically aligned with these metabolic impairments.44
What does the future hold?
As clinicians and researchers, we cannot continue to do the same thing and expect a different result. Given a single change in the sensorimotor system, such as altered sensory afference after ACLR, the CNS must change incrementally throughout its distributed network in a way that maintains the key features of behavior (i.e., balance, gait, etc.). Our historical response to treat the muscle as disconnected from the sensorimotor system is failing us.
The complexity of the CNS makes it incredibly difficult to know where to intervene. But we must not be afraid to try. Changes to the CNS are not hardwired and the potential for inducing long-term neuroplastic change has been demonstrated in populations with far greater denervation (i.e., stroke, spinal cord injury). The future of ACL injury rehabilitation must consider interventions which guide beneficial neuroplasticity through neuromodulation. Going forward, a global appreciation of the embodied sensorimotor system will be required to legitimately test these theories in a systematic scientific manner. This will require diverse neurophysiological and neurochemical assessments, the most impactful of which will incorporate clinician expertise, consider the patient experience, and utilize accessible modalities.
Areas where we need a deeper understanding are interpersonal dynamics, neural network changes, reactive motor control, and guidance for psychological, social, and contextual factors. For now, interventions that induce beneficial plasticity by targeting spinal reflexive excitability, sensorimotor re-weighting, visuomotor dependency, corticospinal excitability, and local muscle growth factors exist and should be applied!
Dave's Reading List
Lisee, et al.’s qualitative synthesis of psychological responses to ACLR.
Needle, Lepley, & Grooms’ review of the neural impacts of ligament injuries.
Rice & McNair’s review of treatments for quadriceps arthrogenic muscle inhibition.
Santos et al.’s discussion of interpersonal coordination in soccer.
Reach out to Dave on Twitter with follow-up questions or to discuss/debate these points. He is always looking to draw from others’ clinical experiences and grow his network.
References:
Griffin LY, Agel J, Albohm MJ, et al. Noncontact anterior cruciate ligament injuries: risk factors and prevention strategies. J Am Acad Orthop Surg. 2000;8(3):141-150.
Gupta AS, Pierpoint LA, Comstock RD, Saper MG. Sex-Based Differences in Anterior Cruciate Ligament Injuries Among United States High School Soccer Players: An Epidemiological Study. Orthopaedic journal of sports medicine. 2020;8(5):2325967120919178-2325967120919178.
Santos R, Duarte R, Davids K, Teoldo I. Interpersonal Coordination in Soccer: Interpreting Literature to Enhance the Representativeness of Task Design, From Dyads to Teams. Front Psychol. 2018;9:2550.
Gibson JJ. The ecological approach to visual perception. 1979.
Brooks JX, Cullen KE. Predictive Sensing: The Role of Motor Signals in Sensory Processing. Biol Psychiatry Cogn Neurosci Neuroimaging. 2019;4(9):842-850.
Wolpert DM, Flanagan JR. Motor prediction. Curr Biol. 2001;11(18):R729-R732.
Straka H, Simmers J, Chagnaud BP. A New Perspective on Predictive Motor Signaling. Curr Biol. 2018;28(5):R232-R243.
Diekfuss JA, Grooms DR, Yuan W, et al. Does brain functional connectivity contribute to musculoskeletal injury? A preliminary prospective analysis of a neural biomarker of ACL injury risk. J Sci Med Sport. 2019;22(2):169-174.
Kiefer AW, Ford KR, Paterno MV, et al. Inter-segmental postural coordination measures differentiate athletes with ACL reconstruction from uninjured athletes. Gait Posture. 2013;37(2):149-153.
Paterno MV, Kiefer AW, Bonnette S, et al. Prospectively identified deficits in sagittal plane hip-ankle coordination in female athletes who sustain a second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. Clin Biomech (Bristol, Avon). 2015;30(10):1094-1101.
Moraiti CO, Stergiou N, Ristanis S, et al. The effect of anterior cruciate ligament reconstruction on stride-to-stride variability. Arthroscopy. 2009;25(7):742-749.
Riemann BL, Lephart SM. The sensorimotor system, part I: the physiologic basis of functional joint stability. J Athl Train. 2002;37(1):71-79.
Kandel ER, Mack S. Principles of neural science. 2014.
Johansson H, Sjolander P, Sojka P. A sensory role for the cruciate ligaments. Clin Orthop Relat Res. 1991(268):161-178.
Courtney CA, Rine RM. Central somatosensory changes associated with improved dynamic balance in subjects with anterior cruciate ligament deficiency. Gait Posture. 2006;24(2):190-195.
Ochi M, Iwasa J, Uchio Y, Adachi N, Sumen Y. The regeneration of sensory neurones in the reconstruction of the anterior cruciate ligament. J Bone Joint Surg Br. 1999;81(5):902-906.
Sonnery-Cottet B, Saithna A, Quelard B, et al. Arthrogenic muscle inhibition after ACL reconstruction: a scoping review of the efficacy of interventions. Br J Sports Med. 2018.
Gokeler A, McKeon PO, Hoch MC. Shaping the Functional Task Environment in Sports Injury Rehabilitation: A Framework to Integrate Perceptual-Cognitive Training in Rehabilitation. Athletic Training & Sports Health Care. 2020;12(6):283-292.
Swanik CB, Covassin T, Stearne DJ, Schatz P. The relationship between neurocognitive function and noncontact anterior cruciate ligament injuries. Am J Sports Med. 2007;35(6):943-948.
Guo Z, Li A, Yu L. "Neural Efficiency" of Athletes' Brain during Visuo-Spatial Task: An fMRI Study on Table Tennis Players. Front Behav Neurosci. 2017;11:72.
Cross ES, Schmitt PJ, Grafton ST. Neural substrates of contextual interference during motor learning support a model of active preparation. J Cogn Neurosci. 2007;19(11):1854-1871.
Dunst B, Benedek M, Jauk E, et al. Neural efficiency as a function of task demands. Intelligence. 2014;42(100):22-30.
Medina D, Barraza P. Efficiency of attentional networks in musicians and non-musicians. Heliyon. 2019;5(3):e01315.
Yang C, Luo N, Liang M, et al. Altered Brain Functional Connectivity Density in Fast-Ball Sports Athletes With Early Stage of Motor Training. Front Psychol. 2020;11:530122.
Bishop DT, Wright MJ, Jackson RC, Abernethy B. Neural bases for anticipation skill in soccer: an FMRI study. J Sport Exerc Psychol. 2013;35(1):98-109.
Orgs G, Dombrowski J-H, Heil M, Jansen-Osmann P. Expertise in dance modulates alpha/beta event-related desynchronization during action observation. Eur J Neurosci. 2008;27(12):3380-3384.
Criss CR, Onate JA, Grooms DR. Neural activity for hip-knee control in those with anterior cruciate ligament reconstruction: A task-based functional connectivity analysis. Neurosci Lett. 2020;730:134985.
Wulf G, Lewthwaite R. Optimizing performance through intrinsic motivation and attention for learning: The OPTIMAL theory of motor learning. Psychon Bull Rev. 2016;23(5):1382-1414.
Gokeler A, Neuhaus D, Benjaminse A, Grooms DR, Baumeister J. Principles of Motor Learning to Support Neuroplasticity After ACL Injury: Implications for Optimizing Performance and Reducing Risk of Second ACL Injury. Sports Med. 2019.
Diekfuss JA, Bonnette S, Hogg JA, et al. Practical Training Strategies to Apply Neuro-Mechanistic Motor Learning Principles to Facilitate Adaptations Towards Injury-Resistant Movement in Youth. Journal of Science in Sport and Exercise. 2020.
Bonnette S, Diekfuss JA, Grooms DR, et al. Electrocortical dynamics differentiate athletes exhibiting low- and high- ACL injury risk biomechanics. Psychophysiology. 2020:e13530.
Diekfuss JA, Grooms DR, Bonnette S, et al. Real-time biofeedback integrated into neuromuscular training reduces high-risk knee biomechanics and increases functional brain connectivity: A preliminary longitudinal investigation. Psychophysiology. 2020;57(5):e13545.
Truong LK, Mosewich AD, Holt CJ, Le CY, Miciak M, Whittaker JL. Psychological, social and contextual factors across recovery stages following a sport-related knee injury: a scoping review. Br J Sports Med. 2020.
Lisee CM, DiSanti JS, Chan M, et al. Gender Differences in Psychological Responses to Recovery After Anterior Cruciate Ligament Reconstruction Before Return to Sport. J Athl Train. 2020.
Burland JP, Lepley AS, Cormier M, DiStefano LJ, Lepley LK. Examining the Relationship Between Neuroplasticity and Learned Helplessness After ACLR: Early Versus Late Recovery. J Sport Rehabil. 2020:1-8.
McPherson AL, Feller JA, Hewett TE, Webster KE. Psychological Readiness to Return to Sport Is Associated With Second Anterior Cruciate Ligament Injuries. Am J Sports Med. 2019;47(4):857-862.
Rush JL, Glaviano NR, Norte GE. Assessment of Quadriceps Corticomotor and Spinal-Reflexive Excitability in Individuals with a History of Anterior Cruciate Ligament Reconstruction: A Systematic Review and Meta-analysis. Sports Med. 2021.
Lepley AS, Ly MT, Grooms DR, Kinsella-Shaw JM, Lepley LK. Corticospinal tract structure and excitability in patients with anterior cruciate ligament reconstruction: A DTI and TMS study. Neuroimage Clin. 2020;25:102157.
Scheurer SA, Sherman DA, Glaviano NR, Ingersoll CD, Norte GE. Corticomotor function is associated with quadriceps rate of torque development in individuals with ACL surgery. Exp Brain Res. 2020;238(2):283-294.
Gabler C, Kitzman PH, Mattacola CG. Targeting quadriceps inhibition with electromyographic biofeedback: a neuroplastic approach. Crit Rev Biomed Eng. 2013;41(2):125-135.
Grospretre S, Lebon F, Papaxanthis C, Martin A. New evidence of corticospinal network modulation induced by motor imagery. J Neurophysiol. 2016;115(3):1279-1288.
Lepley LK, Davi SM, Burland JP, Lepley AS. Muscle Atrophy After ACL Injury: Implications for Clinical Practice. Sports Health. 2020:1941738120944256.
Lisee C, Lepley AS, Birchmeier T, O'Hagan K, Kuenze C. Quadriceps strength and volitional activation after anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Sports Health. 2019;11(2):163-179.
Lambert B, Hedt CA, Jack RA, et al. Blood Flow Restriction Therapy Preserves Whole Limb Bone and Muscle Following ACL Reconstruction. Orthopaedic Journal of Sports Medicine. 2019;7(3_suppl2):2325967119S2325900196.